Healthcare Revenue Cycle Management Market Size and Companies
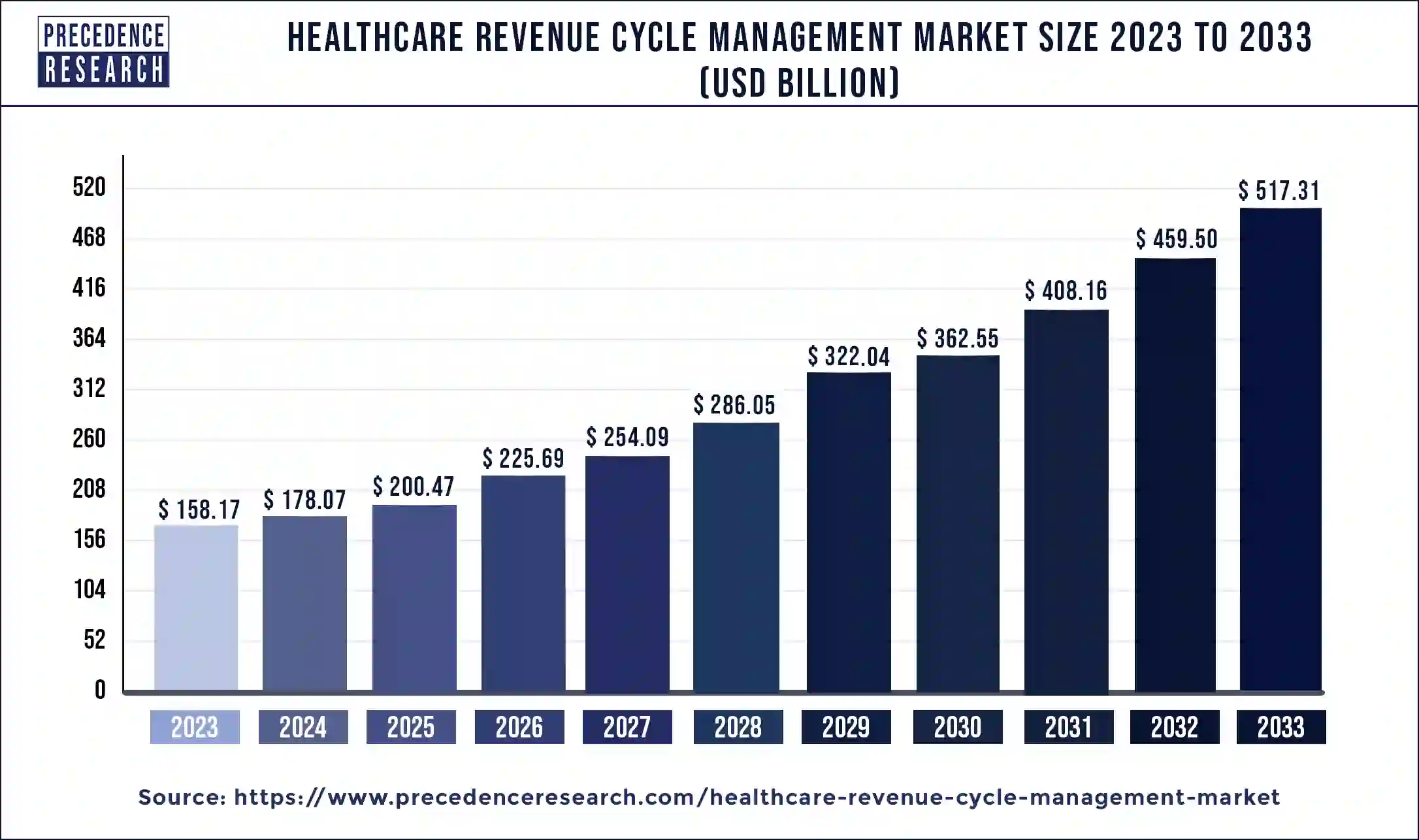
The global healthcare revenue cycle management market size reached USD 158.17 Billion in 2023 and is expected to hit around USD 517.31 billion by 2033, growing at a CAGR of 12.58% from 2024 to 2033. Healthcare revenue cycle management is helpful for the quality of patient care and healthcare organizations' financial stability.
Healthcare Revenue Cycle Management Market Key Takeaways
- The global healthcare revenue cycle management market was valued at USD 178.07 billion in 2024.
- It is projected to reach USD 517.31 billion by 2034.
- The market is expected to grow at a CAGR of 12.58% from 2025 to 2034.
- The global healthcare revenue cycle management market size accounted for USD 75.92 billion in 2023 and is expected to rise around USD 248.31 billion by 2033
- North America dominated the market with the largest market share of 48% in 2023.
- Asia Pacific is estimated to be the fastest-growing during the forecast period of 2024-2033.
- By product type, the integrated segment has contributed more than 82% of market share in 2023.
- By function type, the claims & denial management segment dominated the market in 2023.
- By function type, the medical coding and billing segment is expected to be the fastest growing during the forecast period.
- By deployment type, the cloud-based segment has held the largest market share of 70% in 2023.
- By end-user, the physician office segment dominated the market in 2023.
Healthcare Revenue Cycle Management Market Size in the U.S. 2024 to 2033
The U.S. healthcare revenue cycle management market size was estimated at USD 56.94 billion in 2023 and is predicted to be worth around USD 187.47 billion by 2033, at a CAGR of 12.65% from 2024 to 2033.
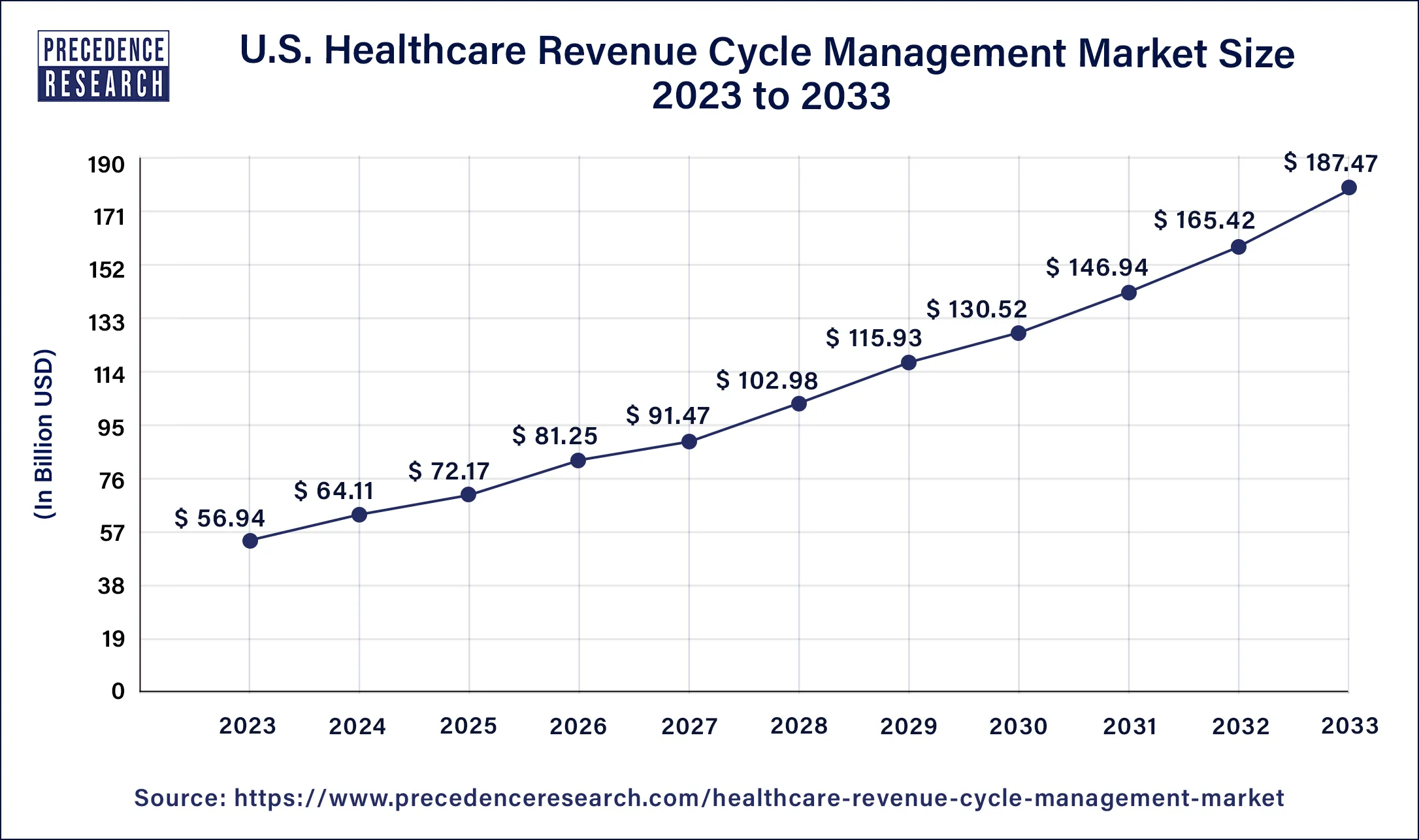
North America dominated the healthcare revenue cycle management market in 2023. Increasing chronic diseases and the senior population have led to the growth of the market in the North American region. Increasing use of cloud-based solutions and electronic health records. Investments in two types of North American healthcare IT companies of healthcare revenue cycle management include AI tools and digital health platforms, which contribute to the growth of the market in this region. The U.S. healthcare environment demands a radically reimagined healthcare revenue cycle management, which is one that is highly manual and transactional. This healthcare revenue cycle management helps healthcare organizations evolve patient expectations and create an increasingly data-rich ecosystem, which helps the growth of the market.
- In September 2023, Integrated RCM Services was launched in the U.S. to provide third-party billing for behavioral providers. It is helpful for patient eligibility, data management, benefits payment posting, billing, audits, coding, verification, account receivable follow-ups, patient balance management, denial management, and insights and analytics.
- In February 2024, a new resource hub for non-clinical AI use in healthcare to help healthcare professionals was launched by the American Health Information Management Association (AHIMA). This tool supports healthcare revenue cycle management, operations, clinical care, and health information management.
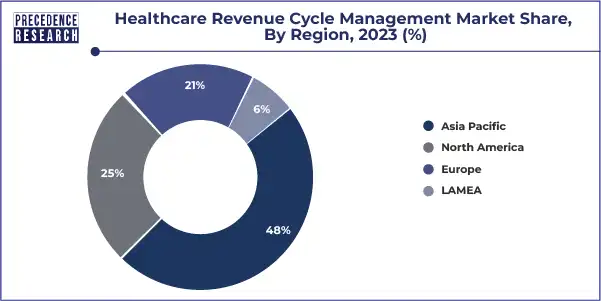
Asia Pacific is estimated to be the fastest-growing during the forecast period of 2024-2033. Increasing patients, rising demand for effective healthcare services, and increase in health insurance help the growth of the market in this region. These factors contribute to the growth of the healthcare revenue cycle management market in the Asia Pacific region. Better software systems are being adopted in countries like China, Japan, South Korea, and India, and revenue management systems are being integrated into the healthcare industries of developing countries.
Healthcare Revenue Cycle Management Market Size in the North America 2024 to 2033
The Asia Pacific healthcare revenue cycle management market size was calculated at USD 33.22 billion in 2023 and is estimated to surpass USD 111.22 billion by 2033. at a CAGR of 12.84% from 2024 to 2033
| Year | Market Size (USD Billion) |
| 2023 | 33.22 |
| 2024 | 37.39 |
| 2025 | 42.10 |
| 2026 | 47.39 |
| 2027 | 53.36 |
| 2028 | 60.07 |
| 2029 | 67.63 |
| 2030 | 76.14 |
| 2031 | 85.71 |
| 2032 | 96.50 |
| 2033 | 111.22 |
Healthcare Revenue Cycle Management Market Overview
The financial procedures used by healthcare institutions to oversee the clinical and administrative tasks involved in the processing, payment, and creation of revenue from claims are known as healthcare revenue cycle management. The healthcare revenue cycle management market deals with medical services, and the process consists of identifying, managing, and collecting patient service revenue. Healthcare revenue cycle management has many benefits, including helping increase operational efficiency, care for patients, improve billing and collections processes, reduce errors in the healthcare authorization process, and help healthcare organizations get paid for patient services. Healthcare revenue cycle management also helps to reduce waste of resources, to support better patient engagement, and to reduce excess costs through a reduced administrative burden. It may have a remarkable positive effect on healthcare practice's patient satisfaction, financial success, and efficiency. Preventing claim denials, optimizing revenue practices and collections, and streamlining administrative tasks can help to enhance healthcare revenue and decrease administrative burdens.
Healthcare Revenue Cycle Management Market Growth Factors
- Healthcare revenue cycle management helps to reduce costs, reduces patient fraud, reduces healthcare fraud, reduces overtreatment, reduces denials, reduces errors, decreases administrative burdens, and saves staff time, which contributes to the growth of the healthcare revenue cycle management market.
- This management helps to increase revenue, increase patient experience with healthcare organizations, improve patient care, speed up revenue collection processes, simplify processes, increase organizational efficiency, increase claims when paid on the first submission, and help to point out missing information of the patient chart.
- It helps healthcare organizations gain a better understanding of all their revenue collection processes and insurance authorization. It also helps healthcare providers transform to asset-based reimbursement practices.
- It allows greater visibility of process inefficiencies and problems. These factors help to the growth of the healthcare revenue cycle management market.
Healthcare Revenue Cycle Management Market Scope
| Report Coverage | Details |
| Growth Rate from 2024 to 2033 | CAGR of 12.58% |
| Global Market Size in 2023 | USD 158.17 Billion |
| Global Market Size in 2024 | USD 178.07 Billion |
| Global Market Size by 2033 | USD 517.31 Billion |
| Largest Market | North America |
| Base Year | 2023 |
| Forecast Period | 2024 to 2033 |
| Segments Covered | By Product Type, By Function Type, By Deployment Type, and By End-user |
| Regions Covered | North America, Europe, Asia-Pacific, Latin America, and Middle East & Africa |
Healthcare Revenue Cycle Management Market Dynamics
Driver
Reduced costs and delays linked with denied claims
Healthcare facilities have a number of expenses to consider, including staff payment for their work and the services they provide to patients. When patients are unable to pay for services or when claims are denied, then healthcare facilities' payments are delayed, and this is a challenging practice for managing expenses. Healthcare revenue cycle management helps to identify claim denial patterns and allows timely reimbursement to be received to avoid future claim denials. It helps organizations in claims denial management by providing needed information and reducing errors. Healthcare revenue cycle management helps to increase efficiencies and simplify processes and also helps to reduce administrative work and errors, which leads to cost reduction for healthcare organizations. These factors help to the growth of the healthcare revenue cycle management market.
Restraint
High implementation costs and difficulty of integration
Implementation of healthcare cycle management revenue cycle management may be costly. It includes potential workflow adjustments, cost of software, and training staff. For smaller healthcare providers, it may be challenging to justify costs upfront. It requires too many resources to manage the healthcare revenue cycle and may cause unacceptable errors. In the meantime, healthcare revenue cycle management solutions may not allow integration or customization with EMR data and payer. These factors restrict the growth of the healthcare revenue cycle management market.
Opportunities
Artificial intelligence and automation
Advancements in artificial intelligence (AI) and automation are transforming the way healthcare revenue cycle management is managed. AI-powered tools may operate automatically and perform repetitive tasks, including increasing efficiency, reducing manual errors, eligibility verification, and claims processing. Artificial intelligence algorithms may analyze large amounts of data and also provide valuable awareness for healthcare revenue cycle management optimization. These factors help to grow the healthcare revenue cycle management market.
Improved mobile solutions for payments and billing
In the healthcare sector, mobile payments and billing have become popular. With the worldwide use of mobile phones or smartphones, patients expect seamless and convenient payment and billing options. Mobile payment gateways and apps allow patients to view statements, pay bills, and set up payment plans, improving collections and reducing account receivables. These factors contribute to the growth of the healthcare revenue cycle management market.
Acceptance of remote patient monitoring and telehealth
Remote patient monitoring and telehealth have gained remarkable progress nowadays and are expected to grow continuously in the future. These technologies permit healthcare providers to expand their gain, remotely provide care, and monitor patients' health conditions. By the implementation of telehealth into healthcare revenue cycle management, healthcare organizations may optimize the reimbursement process and billing process for virtual healthcare services. These factors help to the growth of the market.
Product Type Insights
The integrated segment dominated the market in 2023, and it is also expected to be the fastest-growing during the forecast period. Integrated healthcare revenue belongs to an integrated approach that incorporates all the administrative and financial processes involved in the healthcare revenue cycle management into the integrated system. It involves the integration of many functions, including patient collections, payment processing, claims management, billing, coding, scheduling, and registration, to optimize and streamline healthcare revenue cycle management.
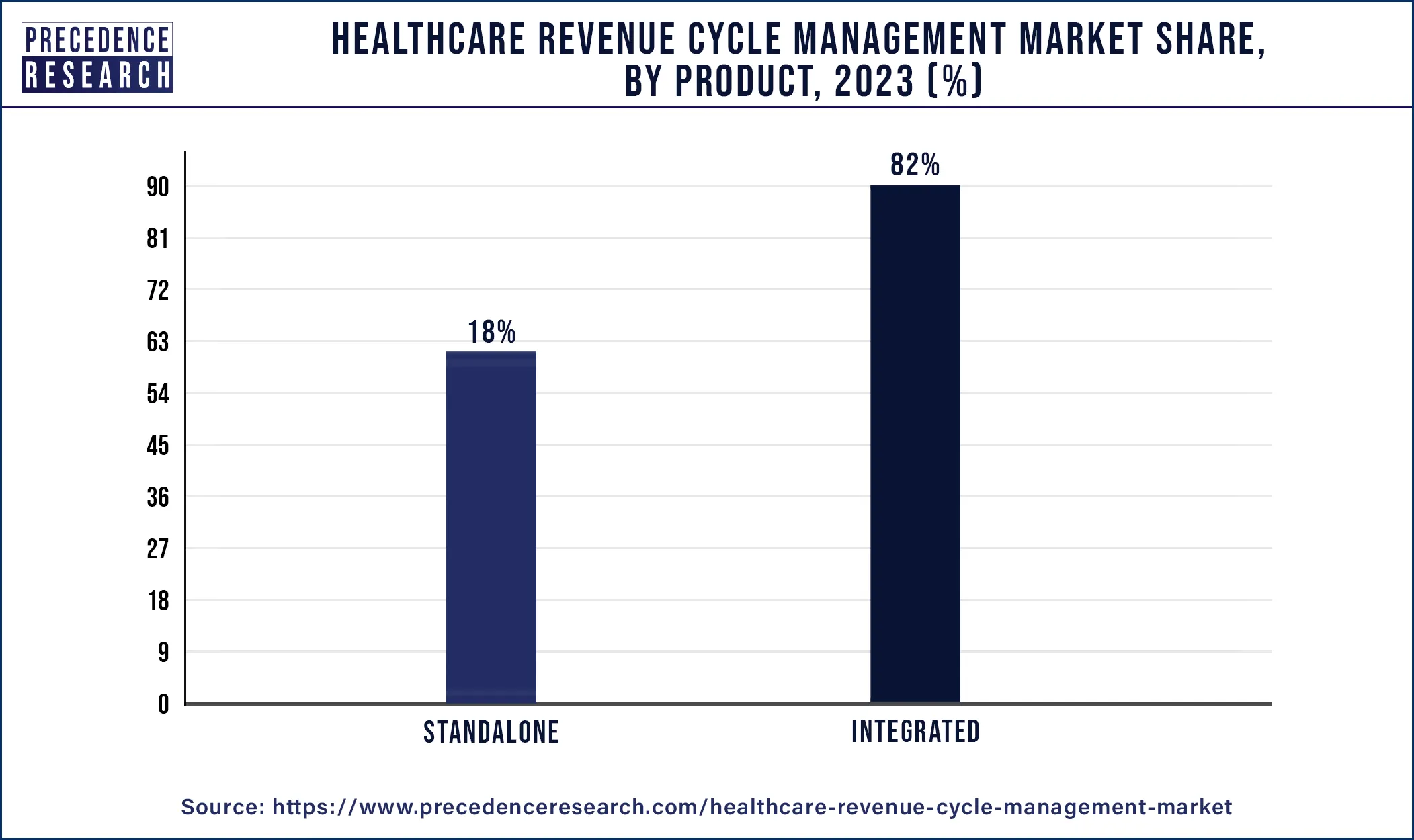
The integrated system helps to improve healthcare providers' financial performance by improving efficiency, maximizing revenue capture, minimizing errors, and reducing costs. By automating and integrating the healthcare revenue cycle management process, an integrated system permits improved decision-making capabilities, real-time visibility, and perfect data flow, which leads to better patient care and improved financial outcomes. These factors of the integrated system help the growth of the segment and contribute to the growth of the healthcare revenue cycle management market.
Function Type Insights
The claims & denial management segment dominated the market in 2023. Providers can handle claim rejections more methodically by using a denial management strategy known as the IMMP process, which stands for Identify, Manage, Monitor, and Prevent. Claim denials in healthcare can be caused by missing or incorrect patient information, coding errors, untimely filing, duplicate claims, missing authorization, or dual coverage issues. Accurate medical billing and coding are crucial to avoid coding errors and claim denials. Pre-authorization for medical procedures is usually required, and timely filing is necessary to avoid claim denials. Dual coverage issues can complicate the claims process, especially when there is a dispute with one or both insurers. Monitoring performance indicators, examining billers and payers, searching for denial management in healthcare trends, figuring out the root reasons, streamlining workflows, and taking proactive measures to stop rejections are all part of claims denial management. Denial management is an ongoing endeavor to strengthen your revenue cycle, especially in light of the fact that payer rules and the reasons for rejections are continually changing. Sustaining a sustainable financial position in the healthcare industry requires a proactive approach to denial management. Effective denial management enables firms to take remedial action that may permanently stop rejections from occurring in the future by identifying the underlying reason for denied claims.
The medical coding and billing segment is expected to grow the fastest during the forecast period. An effective healthcare revenue cycle management must have specific medical coding and billing. Both patients and healthcare professionals benefit from effective medical coding and billing. Healthcare revenue cycle management helps with coding accuracy and productivity. The medical coding process helps to collect, manage, and record patient service revenue for healthcare organizations. Medical coding is the standard way for sharing and documenting the services and treatments provided to the patients. Effective healthcare revenue cycle management acts as a base for successful financial sustainability and medical billing. Healthcare revenue cycle management is essential for medical billing due to improved patient satisfaction, improved revenue generation, reduced billing errors, and improved cash flow. These factors help to the growth of the segment and contribute to the growth of the healthcare revenue cycle management market.
Deployment Type Insights
The cloud-based segment dominated the market in 2023, and it is expected to grow the fastest during the forecast period. Cloud-based healthcare revenue cycle management is highly used because it provides accessibility, scalability, and costs.
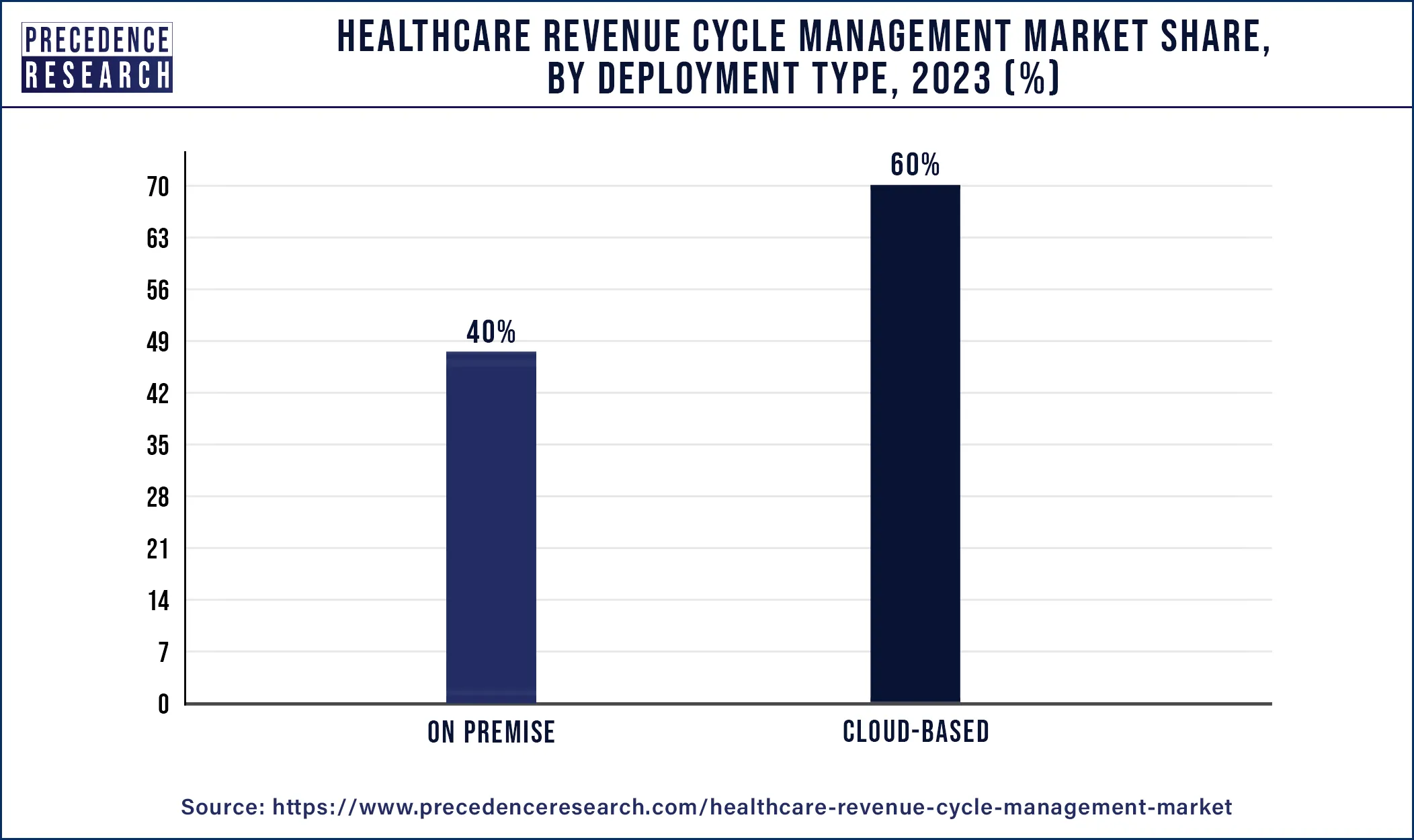
Cloud has many benefits, including data privacy and security, in healthcare IT departments and other areas of operations. Using cloud-based deployment to align costs to healthcare revenue cycle management better creates good financial health. Cloud-based deployment offers many benefits for healthcare systems. These factors help to the growth of the segment and contribute to the growth of the healthcare revenue cycle management market.
End-user Insights
The physician office segment dominated the healthcare revenue cycle management market in 2023. Physician healthcare revenue cycle management is a financial process that improves healthcare practices to track the healthcare revenue cycle management of patients from their initial consultation or appointments to the final payment balance. It is an essential part of medical billing and is concerned with payment management. It helps to ensure claims are processed accurately and quickly and improves healthcare revenue cycle management. The physician office end-user type is helpful for a healthy healthcare revenue cycle for providing high-quality care with a sustainable business model. It helps to reduce errors in the billing process, improves financial health practices, and maintains regulatory compliance. It also helps in patients' collection and billing, payment reconciliation and posting, claim submission and charge capture, insurance verification and insurance eligibility, patient registration, and patient scheduling. It also helps in sustainability growth driving. These factors help to the growth of the physician office end-user segment and contribute to the growth of the market.
Healthcare Revenue Cycle Management Market Recent Developments
- In March 2022, a new solution at HIMSS22 was announced by healthcare vendors' software companies, including tools to enhance patient billing processes and end-to-end revenue cycle management platforms.
- In October 2023, a technology-enabled solution, Omega Healthcare, launched Omega Digital Platform (ODP) to help healthcare organizations improve healthcare revenue cycle outcomes, improve financial performance, and reduce administrative burdens.
- In October 2023, a Revenue Management Firm was launched by Dignity Health, Optum. A large West Coast healthcare system has joined with a healthcare IT firm. It formed Optum 360, which aimed to help hospitals optimize revenues and prepare for new methods of payments.
- In December 2023, the revenue cycle management technology adoption model (RCMTAM) was launched by a healthcare revenue cycle management Fin Thrive, Inc., and the Healthcare Financial Management Association (HFMA).
Healthcare Revenue Cycle Management Market Companies
- Allscripts Healthcare, LLC
- Dell Technologies
- Athenahealth
- AGS Health Inc.
- Experion Information Solutions, Inc.
- CareCloud, Inc.
- Cerner Corporation
- Change Healthcare
- Cognizant
- Conifer Health Solutions, LLC.
- Medical Information Technologies, Inc.
- McKesson Corporation
- Optum
- R1 RCM, Inc.
- SSI Group Formativ Health
Segments Covered in the Report
By Product Type
- Integrated
- Standalone
By Function Type
- Claims and Denial Management
- Medical Coding and Billing
- Eligibility Verification
- Payment Remittance
- Others
By Deployment Type
- On-premise
- Cloud-based
By End-user
- Hospitals
- Physician Office
- Diagnostic Labs and Ambulatory Surgical Centers
- Others
By Geography
- North America
- Europe
- Asia Pacific
- Latin America
- Middle East and Africa
For inquiries regarding discounts, bulk purchases, or customization requests, please contact us at sales@precedenceresearch.com
Frequently Asked Questions
Ask For Sample
No cookie-cutter, only authentic analysis – take the 1st step to become a Precedence Research client
 Get a Sample
Get a Sample
 Table Of Content
Table Of Content
 sales@precedenceresearch.com
sales@precedenceresearch.com
 +1 804-441-9344
+1 804-441-9344
 Schedule a Meeting
Schedule a Meeting