Blood Pressure Monitoring Devices Market Size and Forecast 2025 to 2034
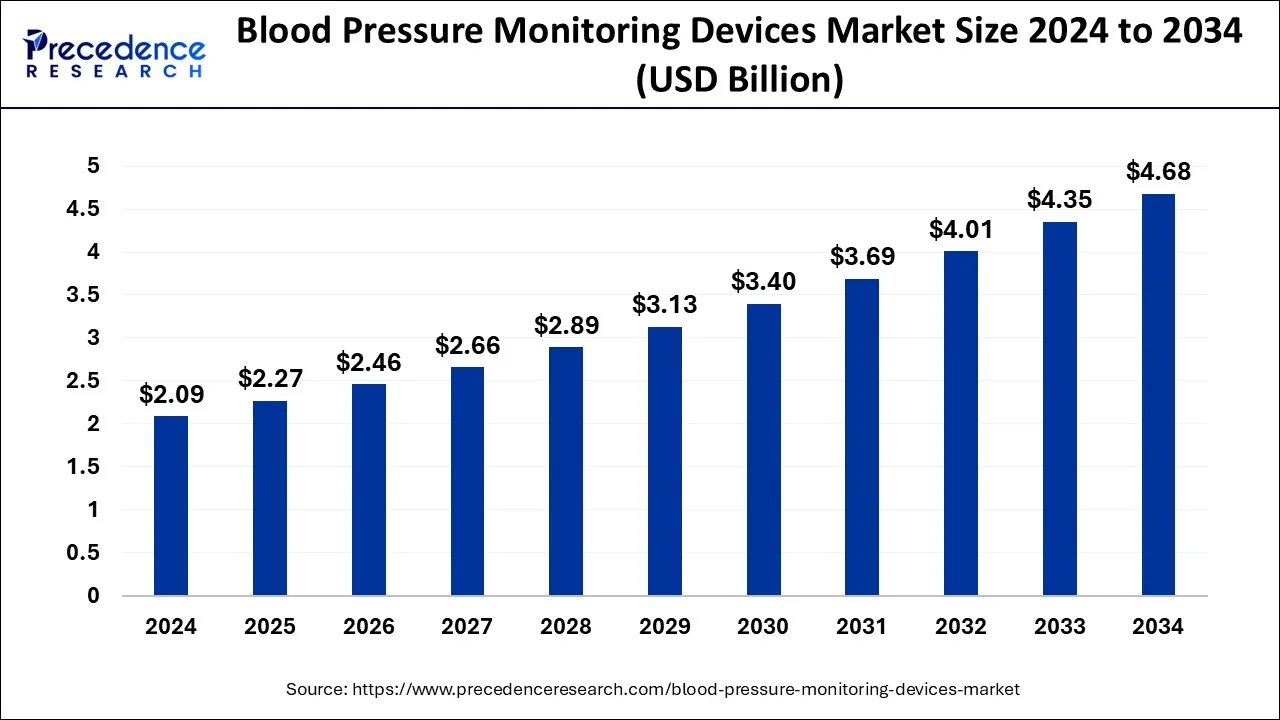
The global blood pressure monitoring devices market size was estimated at USD 2.09 billion in 2024 and is anticipated to reach around USD 4.68 billion by 2034 and is poised to grow at a CAGR of 8.49% during the forecast period 2025 to 2034. Obesity is a leading cause of rising blood pressure, which has increased the usage of blood pressure monitoring devices, ultimately promoting the market's growth.
Blood Pressure Monitoring Devices Market Key Takeaways
- In terms of revenue, the blood pressure monitoring devices market is valued at $2.27 billion in 2025.
- It is projected to reach $4.68 billion by 2034.
- The blood pressure monitoring devices market is expected to grow at a CAGR of 8.49% from 2025 to 2034.
- North America led the global market with the highest market share of 37.44% in 2024.
- By product, the digital blood pressure monitor segment registered a maximum market share of 35.80% in 2024.
- By end-user, the hospitals segment captured the biggest revenue share of 59.34% in 2024.
Integration of AI in the Market
Artificial Intelligence (AI) has the potential to completely transform the healthcare industry, especially in the areas of blood pressure (BP) and vital sign monitoring. Despite their effectiveness, traditional approaches are frequently constrained by their dependence on irregular measurements and the requirement for specialized equipment. A new age of continuous, individualized, and data-driven healthcare is being ushered in by generative AI models, which provide fresh ways to get around these restrictions. AI's ability to provide frequent and simple remote data gathering is one of the most important ways it is revolutionizing vital signs monitoring. In a similar vein, AI-powered blood pressure monitoring is surpassing conventional cuff-based devices and may even do away with the necessity for a wearable.
U.S. Blood Pressure Monitoring Devices Market Size and Growth 2025 to 2034
The U.S. blood pressure monitoring devices market size surpassed USD 670.20 million in 2024 and is predicted to be worth around USD 1388.17 million by 2034, at a CAGR of 7.64% from 2025 to 2034.
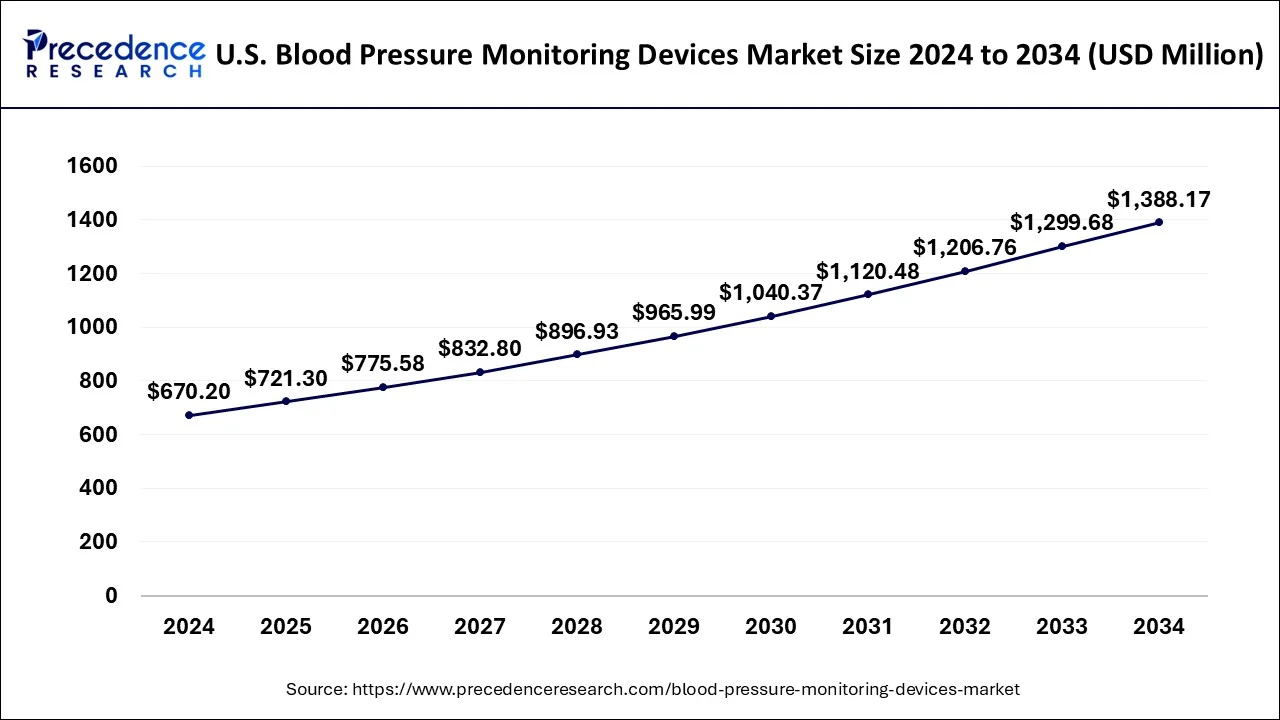
North America led the global blood pressure monitoring devices market with nearly half of the market value share in 2024. This is attributed to the developed healthcare infrastructure along with significant investment for the development of effective and accurate BP monitors in the region.
High blood pressure, often known as hypertension, raises the risk of heart disease and stroke, two of the top causes of mortality in the United States. Clinicians diagnose hypertension in patients and treat them by comparing their systolic and diastolic blood pressure measurements to specific criteria. The hypertension thresholds used by physicians for diagnostic and treatment strategies for patients may range from one clinician to the next:
Canada has been a world leader in hypertension screening, diagnosis, and management for the past two decades. Our national guideline program (which includes our guideline implementation and evaluation teams) has established a global benchmark for evidence-based hypertension care. However, cardiovascular disease remains Canada's greatest cause of death, and we will continue to work hard to prevent, identify, and manage hypertension to improve population cardiovascular health.
Mexico now boasts a population of about 130 million people, with 85 million individuals aged 20 and up. The demographic pyramid continues to have a broader base, which corresponds to persons under the age of 54. Despite projections made 20 years ago that the population pyramid will transition into a mushroom shape as a result of increased life expectancy and adult population growth, this change has not occurred. In Mexico, hypertension has emerged as the most serious noncommunicable chronic disease threat to public health.
Around 30% of the adult Mexican population has hypertension; 75% of them are under the age of 54 (productive age); 40% are unaware, while only 50% of the aware hypertensive population takes medication, and only 50% are under control (140/90 mmHg). Hypertension, dyslipidemia, obesity, and diabetes are all cardiovascular risk factors that frequently coexist in the same person and are amplified by shared pathophysiological pathways.
- In November 2024, Aktiia's continuous blood pressure monitoring (CBPM) bracelet received approval from Health Canada and was launched in the country. It is the company's first market expansion outside of Europe. The company aims to assist millions of people in taking control of their cardiovascular health through continuous and hassle-free monitoring.
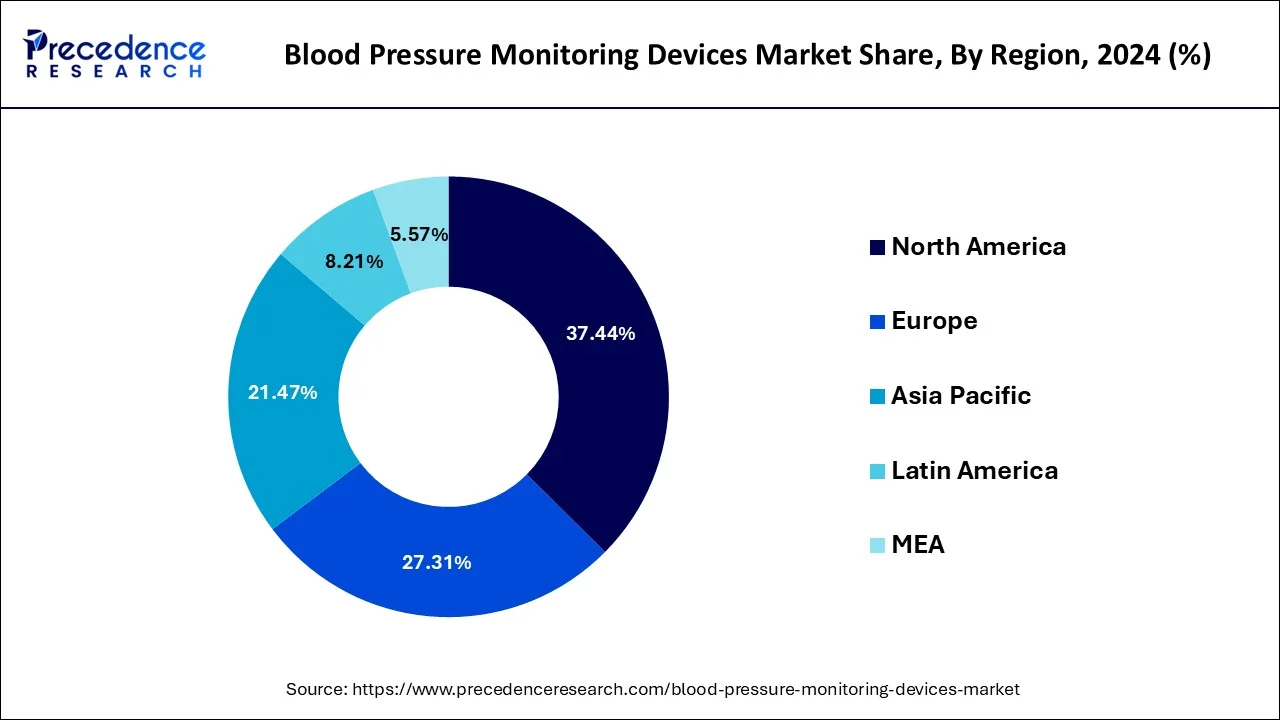
On the contrary, the Asia Pacific shows attractive growth opportunity in the coming years due to rising level health awareness among people, increasing investment from manufacturers, and rising incidences of hypertension. Chronic diseases such as cancer, diabetes, CVDs, and others are becoming more common as the population ages, resulting in a surge in demand for patient monitoring systems. The demand for wearable devices in the region will be driven by an increase in the prevalence of obesity and a growing awareness of fitness and preventative healthcare. Furthermore, the market is expected to rise faster as remote patient monitoring becomes more widely accepted in hospitals.
The remote patient monitoring market is predicted to grow at the fastest rate in Asia Pacific. Growth in the geriatric population, a quick rise in infectious diseases such as SARS (COVID-19), and increased investments by top industry players are some of the primary driving reasons for the remote patient monitoring market. Emerging economies like India and China have a lot of economic potential in the Asia-Pacific area. In nations like India and China, the fast-growing senior population increased awareness of remote patient monitoring, and rising disposable income presents a big market for remote patient monitoring systems.
- India has more than 220 million people who suffer from high blood pressure. In May 2024, OMRON Healthcare India collaborated with AliveCor to launch portable electrocardiogram (ECG) monitoring devices in India. Under this partnership, OMRON Healthcare India offers AI-based handheld ECG technology, besides being a top blood pressure monitor player in India.
Market Overview
Due to the rising aging of the population and the growth in the frequency of chronic diseases, it is projected that the demand for blood pressure monitoring devices will rise globally throughout market analysis. Furthermore, it is anticipated that the rise in healthcare spending in emerging nations and the strong need for proactive monitoring would open up new business prospects for industry participants. Blood pressure monitoring is crucial to assessing the severity of a patient's condition since high blood pressure is also a key cause of a number of illnesses, including heart attacks, strokes, and kidney failure. The rising prevalence of cardiovascular conditions like hypertension, the danger of high blood pressure in the elderly population, and the growing number of lifestyle disorders like diabetes and obesity are the main causes of the rise in the use of blood pressure monitoring devices.
- According to the article published by the CDC in January 2025, High blood pressure increases the risk for heart disease and stroke, which are leading causes of death in the United States. In 2022, high blood pressure was a primary or contributing cause of 685,875 deaths in the United States. Nearly half of adults have high blood pressure (48.1%, 119.9 million). About half of adults (45%) with uncontrolled high blood pressure have a blood pressure of 140/90 mmHg or higher. This includes 37 million U.S. adults.
Blood Pressure Monitoring Devices Market Growth Factors
- Rising cases of hypertension: Rising incidences of hypertension because of changing lifestyles is the key factor counting for the prominent growth of the market during the forecast period.
- Growing old population: Consequently, the demand for Blood Pressure (BP) monitors is very high owing to the growing geriatric population base along with growing risk of lifestyle related disorders among wide population base because of rising incidences of sedentary lifestyle &obesity.
- Government initiatives: Initiatives undertaken by governments of various regions for example public blood pressure (BP) monitoring program for creating awareness amongst people as well as maintain the database created by remotely operated BP monitors predicted to further boost the market growth during the forecast period.
- Growing usage of portable medical devices: Presently, mobiles and wearable & portable devices are gaining popularity due to their associated benefits such as easy handling and the wireless transmission of patient's information.
- Technological advancements: New technologies such as mHealth that support medication & treatment compliances for patients in chronic disease management anticipated to propel the market growth. It helps in tracking the patient's medication schedule, health information, and follow up for the treatment. These related advantages are the key factors projected to augment the overall market growth.
Market Scope
| Report Highlights | Details |
| Market Size in 2024 | USD 2.09 Billion |
| Market Size in 2025 | USD 2.27 Billion |
| Market Size by 2034 | USD 4.68 Billion |
| Growth Rate from 2025 to 2034 | CAGR of 8.49% |
| Largest Market | North America |
| Base Year | 2024 |
| Forecast Period | 2025 to 2034 |
| Segments Covered | By Product Type, and By End-User Type |
| Regions Covered | North America, Europe, Asia-Pacific, Latin America, and Middle East & Africa |
Market Dynamics
Market Drivers
The rising aging population to drive the demand for blood pressure monitoring devices
The world continues to see an extraordinary and long-term shift in the age structure of the global population, owing to rising life expectancy and declining fertility rates.
Women, on average, live longer than men, therefore they make up the bulk of the elderly population, particularly at advanced ages. The number of elderly people worldwide is expected to more than double over the next three decades, reaching over 1.5 billion in 2050. Between 2020 and 2050, the number of elderly will grow in all regions. The proportion of the global population aged 65 and up is predicted to rise from 9.3% in 2020 to roughly 16% in 2050.
Increasing adoption of patient monitoring solutions to drive the demand for BP monitoring devices
HF management has substantial financial ramifications as well. While global estimates are difficult to come by, direct medical expenditures of HF care continue to climb as the disease's prevalence rises. In 2012, $30.7 billion was spent on HF care in the United States, with that figure expected to double by 2030. In many countries, quality programs have moved the financial burden of HF onto health systems, such as the Hospital Readmissions Reduction Program (HRRP) in the United States, where HF readmissions are the leading cause of Medicare reimbursement reductions. Given these clinical and financial reasons, as well as the inadequacies of present methods, considerable work has gone into establishing more effective HF management strategies.
Restraint
Rise in cost due to technological advancements
The commercial expansion of blood pressure measurement equipment is seriously threatened by high costs, which continue to be a major problem. Compared to conventional manual devices, advanced blood pressure monitoring systems have greater starting prices and higher maintenance costs since they integrate digital features and artificial intelligence. Adoption rates may be hampered by this price disparity, particularly for poor groups, smaller clinics, and healthcare institutions.
Opportunity
Remote health monitoring and home-based care
The growing tendency of home care replacing hospital treatment is one of the enduring trends. To meet the needs of homecare patients, most major competitors, including Omron Healthcare, are constantly releasing new blood pressure monitors. The usage of Bluetooth-enabled monitors, which have a long battery life, a small form factor, and the ability to monitor themselves, is another trend. These gadgets guarantee patients receive more comprehensive follow-up treatment and assist in sending patient data to the physician.
- In July 2024, Smart Meter, the leading supplier of Cellular Remote Patient Monitoring (RPM) solutions, unveiled its latest innovative product: the first cellular-connected, multi-cuff blood pressure monitor specifically designed for RPM and chronic care management (CCM).
Product Insights
The digital blood pressure monitor segment emerged as a global leader and accounted for more than 35.80% of value share in the year 2024. Technological advancements along with new product launches anticipated to further augment the demand for sphygmomanometers globally. For example, in January 2017, Omron Healthcare, Inc. introduced Omron EVOLV, a wireless and portable upper arm blood pressure monitoring device. In addition, demand for digital sphygmomanometer projected to expand at lucrative CAGR owing to its associated advantages such as ease of use and accurate results.
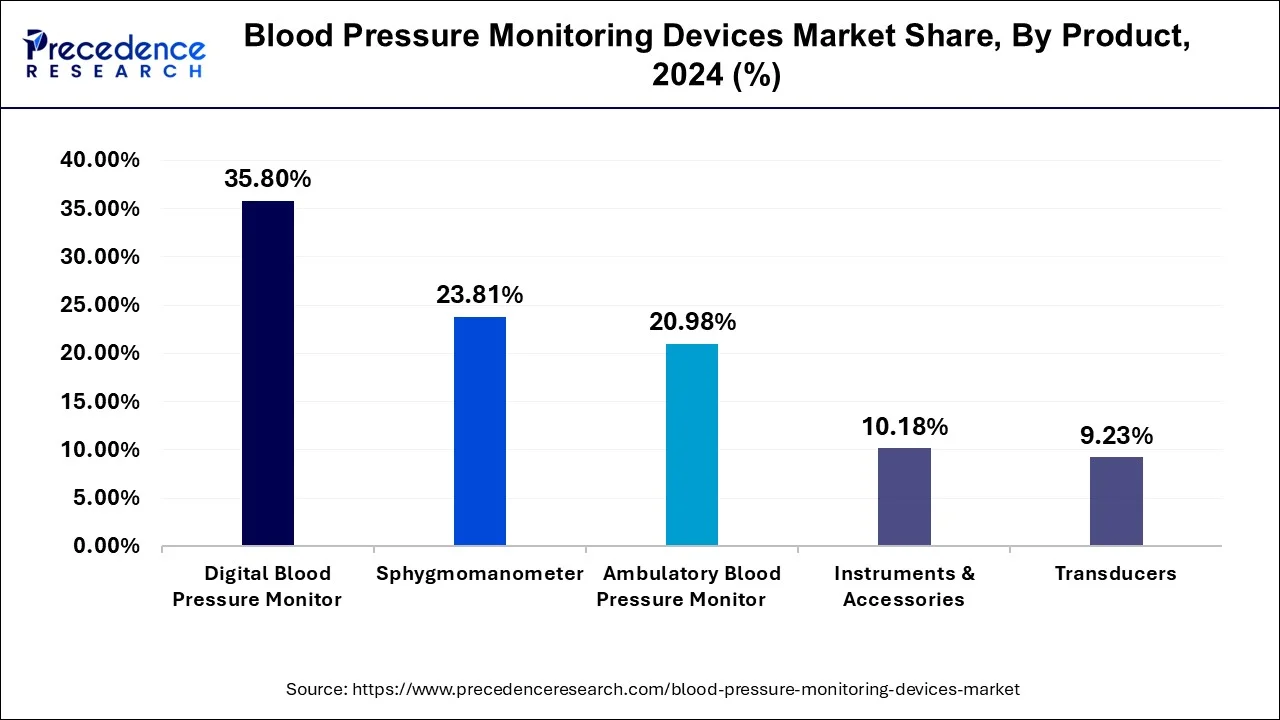
However, blood pressure cuffs anticipated to grow at a rapid rate over the analysis period on account of rising usage of blood pressure monitors backed by the increasing incidences of high blood pressure. These BP cuffs are available in different sizes, as per the type of patients. Basically two types of cuffs are available in the market that includes reusable and disposable. Amongst them, the disposable cuff segment anticipated to register the highest CAGR due to rising adoption of ecofriendly products coupled with the increasing concern about cross-contamination events at hospitals.
Global Blood Pressure Monitoring Devices Market Revenue, By Product, 2021-2023 (USD Million)
| By Product | 2021 | 2022 | 2023 |
| Digital Blood Pressure Monitor | 577.1 | 631 | 689.2 |
| Sphygmomanometer | 400.6 | 428.8 | 458.4 |
| Ambulatory Blood Pressure Monitor | 333.8 | 367.4 | 403.8 |
| Transducers | 149.4 | 163 | 177.7 |
| Instruments & Accessories | 165.1 | 180 | 196 |
End-user Insights
Hospitals segment addressed the largest market value share in the year 2024 attributed to the presence of large patient pool. Further, the rising need for accurate, fast, and effective diagnostic tools for better health outcome anticipated to surge the adoption of BP monitoring devices in the hospital & clinics segment. Rising investment from governments of various regions for the development of hospital & healthcare infrastructure accounts positively towards the growth of BP monitors. Rising investment influence hospital sector to adopt new technologies and devices for early diagnose the problem or disease and cure them.
On the other hand, home healthcare registers the fastest growth of around 12.9% over the analysis period. Increasing availability of smart wearables that provide mobility as well as cost-efficient option for the homecare application is the key factor that drives the overall market growth. Further, increasing cases of high blood pressure along with rising disposable income are the other significant key factors that propel the growth of home healthcare segment.
Blood Pressure Monitoring Devices Market, By End-User Revenue, 2021-2023 (USD Million)
| By End-User | 2021 | 2022 | 2023 |
| Ambulatory Surgical Centers & Clinics | 275.7 | 303.3 | 333.2 |
| Hospitals | 978.5 | 1,057.90 | 1,142.30 |
| Home Healthcare | 371.8 | 409 | 449.5 |
Blood Pressure Monitoring Devices Market Companies
- Koninklijke Philips N.V.
- General Electric Company
- A & D Company, Limited
- SunTech Medical, Inc.
- Welch Allyn
- American Diagnostic Corporation
- Briggs Healthcare
- Withings
- Spacelabs Healthcare
- GF HEALTH PRODUCTS, INC.
- Kaz, A Helen of Troy Company
- Rossmax International Limited
- Microlife Corporation
Recent Developments
- In April 2025, BD launched a surgical monitor with AI-powered blood pressure predictions. BD unveiled a new monitoring platform equipped with AI-powered programs that aim to predict potentially life-threatening changes in the patient's blood pressure during critical procedures.
- In October 2024, Novosound, the Scottish tech company, unveiled the world's first ultrasonic blood pressure monitor. This breakthrough allows for the miniaturization of blood pressure monitoring in wearable devices, including smartwatches and smart rings, achieving accuracy levels comparable to conventional electronic cuff devices.
- In June 2023, Omron Healthcare, a Japan-based manufacturer and distributor of personal healthcare products, announced its plan to set up a medical devices manufacturing plant in Tamil Nadu with an investment of ?128 crore.?A Memorandum of Understanding (MoU) was signed in the presence of the Tamil Nadu Chief Minister, according to a press release from the State government.
- In December 2024, Withings' BPM Pro 2, a cellular blood pressure monitor designed to enhance remote patient care for those with heart failure, has received approval from the U.S. Food and Drug Administration (FDA). The gadget was first introduced in October and went on sale in the United States on January 1 2025.
- In November 2024, in a move that marks the company's first market expansion outside of Europe, Aktiia's continuous blood pressure monitoring (CBPM) wristband was approved by Health Canada and introduced there
Segments Covered in the Report
By Product
- Digital Blood Pressure Monitor
- Wrist
- Arm
- Finger
- Sphygmomanometer
- Ambulatory Blood Pressure Monitor
- Instruments & Accessories
- Blood pressure cuffs
- Reusable
- Disposable
- Others
- Blood pressure cuffs
- Transducers
- Reusable
- Disposable
By End-User
- Ambulatory Surgical Centers & Clinics
- Hospitals
- Home Healthcare
By Geography
- North America
- U.S.
- Canada
- Europe
- U.K.
- Germany
- France
- Asia-Pacific
- China
- India
- Japan
- South Korea
- Malaysia
- Philippines
- Latin America
- Brazil
- Rest of Latin America
- Middle East & Africa (MEA)
- GCC
- North Africa
- South Africa
- Rest of the Middle East & Africa
For inquiries regarding discounts, bulk purchases, or customization requests, please contact us at sales@precedenceresearch.com
Frequently Asked Questions
Ask For Sample
No cookie-cutter, only authentic analysis – take the 1st step to become a Precedence Research client
 Get a Sample
Get a Sample
 Table Of Content
Table Of Content
 sales@precedenceresearch.com
sales@precedenceresearch.com
 +1 804-441-9344
+1 804-441-9344
 Schedule a Meeting
Schedule a Meeting