Pharmacy Benefit Management Market Size and Forecast 2025 to 2034
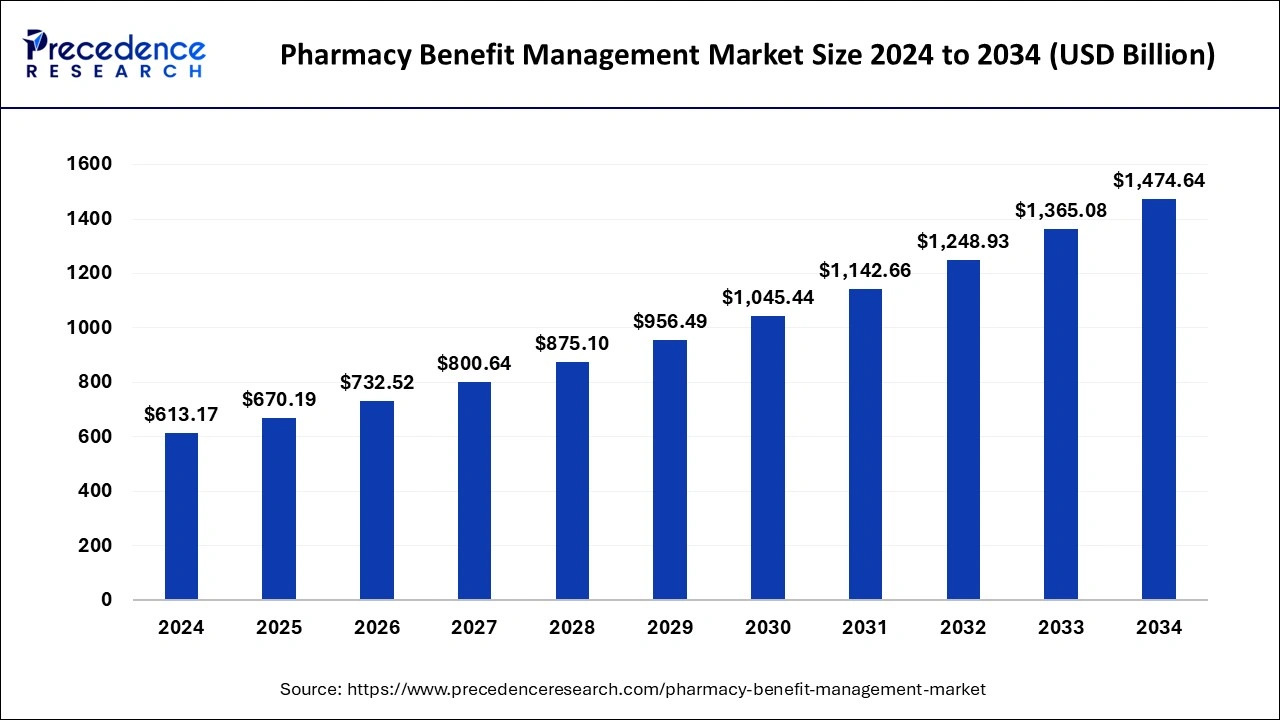
The global pharmacy benefit management market size accounted for USD 613.17 billion in 2024 and is predicted to increase from USD 670.19 billion in 2025 to approximately USD 1,474.64 billion by 2034, expanding at a CAGR of 9.17% from 2025 to 2034
Pharmacy Benefit Management Market Key Takeaways
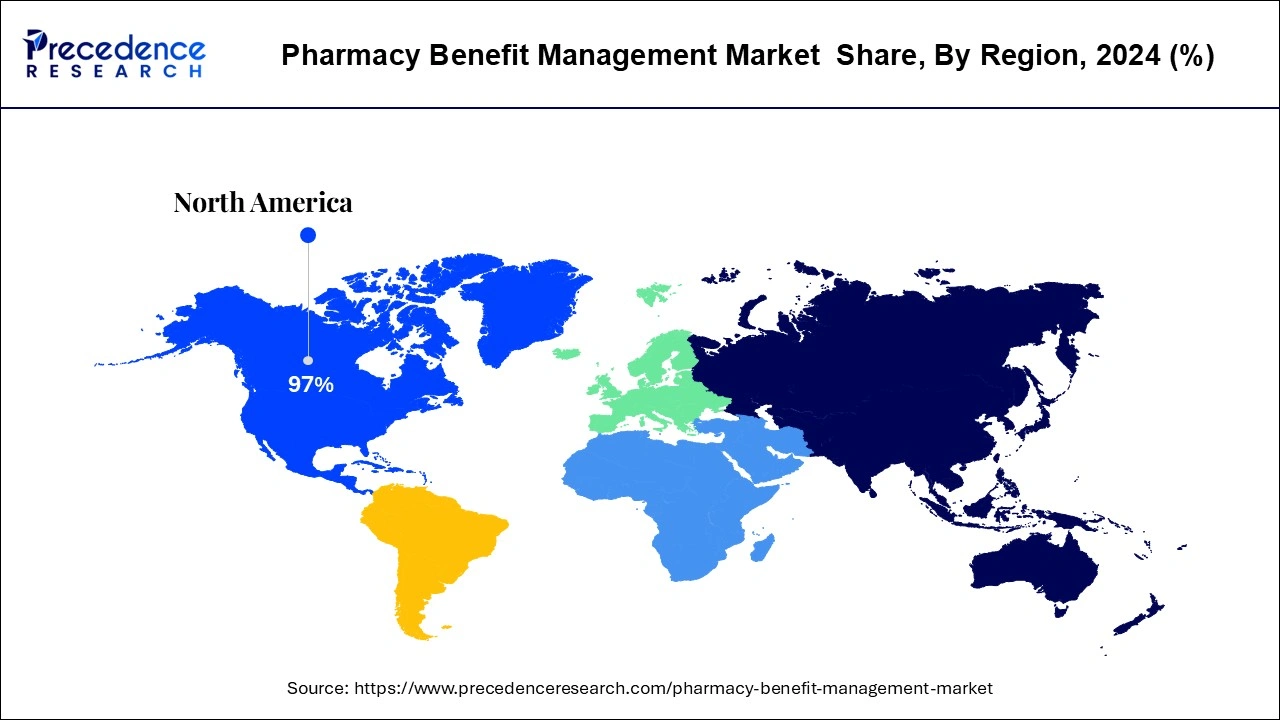
- North America led the global market with the highest market share of 97.14% in 2024.
- Asia Pacific region is estimated to expand the fastest CAGR between 2025 and 2034.
- By Service, the Specialty Pharmacy Services segment has held the largest market share of 34% in 2024.
- By Service Provider, the insurance companies segment captured the biggest revenue share in 2024.
- By Service Provider, the retail pharmacy segment is expected to expand at the fastest CAGR over the projected period.
U.S. Pharmacy Benefit Management Market Size and Growth 2025 to 2034
The U.S. pharmacy benefit management market size was evaluated at USD 419.14 billion in 2024 and is projected to be worth around USD 1,041.11 billion by 2034, growing at a CAGR of 9.53% from 2025 to 2034.
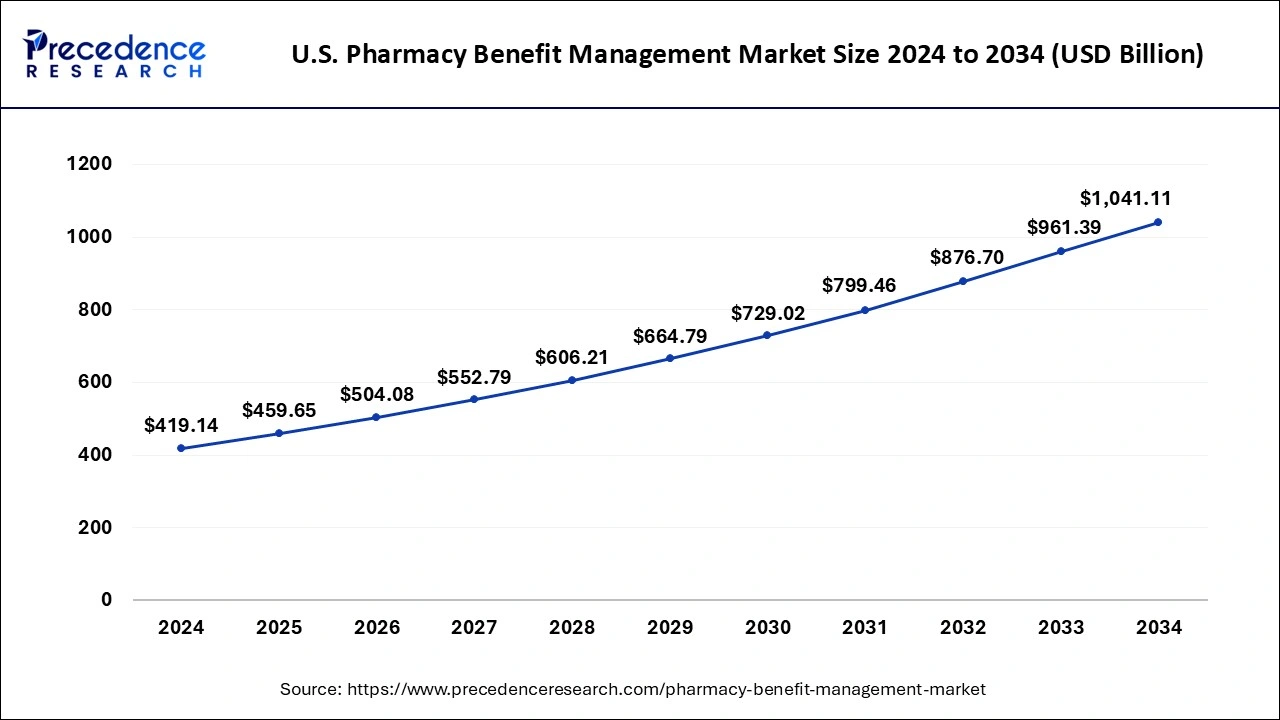
North America dominated the global pharmacy benefit management market in 2024. The US is home to leading pharmaceutical manufacturers, leading insurance providers, leading pharmacy benefit management service providers, and leading retail pharmacy chains. The increased adoption of the health insurances among the US population has supported the market growth. It is estimated that more than half of the US population is suffering from one or more chronic diseases. The high healthcare expenditure and increased adoption of the insurance policies have led to the growth of the North America pharmacy benefit management market. As per the Centers for Medicare and Medicaid Services, the total healthcare expenditure in US increased to US$ 4.1 trillion or an increase of 9.7% in 2020 as compared to the previous year. The huge penetration of the health insurance providers in the region has led to the growth of the North America pharmacy benefit management market. Most of the patients in US depends on the reimbursements for receiving treatment for various diseases. The favorable reimbursement policies of the government have also supported the market growth in North America.
The U.S. solidifies its market lead in Pharmacy Benefit Management (PBM) in North America because of its well-established healthcare system and wide insurance coverage. Major PBM companies such as CVS Caremark, Express Scripts, and OptumRx have well-structured drug pricing negotiations, formulary management, mail order pharmacy services, and government programs. Recent government initiatives aimed to further regulate drug pricing and increase transparency, such as the Inflation Reduction Act, will strengthen the U.S. leadership role.
Asia Pacific is expected to witness a significant growth rate during the forecast period. This is attributed to the rising adoption of the healthcare insurances among the population. The rising prevalence of chronic diseases and rising healthcare expenditure in the region is supporting the market growth. Moreover, the rising penetration of several pharmacy benefit management service providers in the region is expected to boost the growth of the market in the foreseeable future.
In China, a historical shift in the healthcare system, along with the increasing digitalization of the medical record system, and the rapid expansion of private insurance has led to rapid growth and development of the PBM market in China. Centralized drug purchasing and drug price negotiations mandated by the government draw on PBM principles and promote continued growth. Collaborative partners in drug benefit management, and technologies targeting improved medication adherence are increasingly being adopted by insurers and companies. Expanding chronic conditions and urbanization along with the growing demand for cost-effective, technology-based pharmacy services amplify the need for the PBM platform in China.
Market Overview
Pharmacy benefit manager (PBM) specializes as a third-party supervisor. Pharmacy benefit management is an association of drug guides which manages, examines, and manages all the topics in relation with healthcare, and offers advantages of drug programs to the employers. Moreover, it aids in offering management with medical services as well as biologic medications at lowered costs. The cost deduction is attained over refunds with drug producers, coming in agreements with pharmacies, concocting, and remunerating prescription drug alleges and by employing with self-protected associations and government plans. This benefit management liberates the list of medication drugs which involve all drugs enfolded by the name of its advantageous plans, at which point producers are available to provide rebates. PBM is able to be varied and bendable starting from a little, to enormous in size. A few of the sectors of the pharmacy benefit manager involve checking clinical lineups for a vast populace, low price therapeutic alternates, medication therapy management programs & details regarding tablet splitting, and services of mail order.
Pharmacy Benefit Management Market Growth Factors
Pharmacy benefit management refers to the group of companies that act as the middlemen between the insurance companies and drug manufacturers and pharmacies for the purpose of securing lower drug costs for the insurance companies and insurers. The significantly rising prevalence of various chronic diseases among the global population is a primary driver of the global pharmacy benefit management market. The most prominent diseases that constitutes maximum deaths includes cancer, cardiovascular diseases, respiratory diseases, and diabetes. The si8gnificantly rising healthcare costs and healthcare expenditure in the developed and developing nations is boosting the growth of the global pharmacy benefit management market. The rising prevalence of chronic diseases and rising healthcare expenditure is augmenting the demand for the prescription drugs across the globe. This is boosting the demand for the pharmacy benefits management services across the globe.
Furthermore, the rising drug prices across the globe is resulting in increased healthcare spending which is a prominent factor behind the rising demand for the pharmacy benefit management services among the healthcare insurance providers. The rising healthcare expenditure owing to the rising adoption of the expensive drugs for rare diseases is supporting the market growth significantly. The growing penetration of the health insurance providers and rising consumer awareness regarding the benefits of health insurances is expected to boost the demand for the pharmacy benefit management services among the health insurance providers across the globe. The rapid adoption of the pharmacy benefit management services among the drug manufacturers, retail pharmacies, and health insurance providers is shifting the preferences of the service providers towards the advanced workflows that utilizes machine learning technologies. The introduction of the artificial intelligence and machine learning technologies in the pharmacy benefit management services is expected to offer various growth opportunities to the market players.
Growing Advocacy of Machine Learning to Make Regular Workflow
The growing adoption of benefit management services amid the pharmacy links, drug producers, as well as insurance suppliers are changing their propensities of the service suppliers from traditional flow of the work to develop workflow by employing machine learning. As a consequence, associations can offer an exquisite supply chain, speedy mail order delivery and feed to a vast number of coverage and merchandise pharmacy links inside the time limit.
For example, a key player in the U.S., CapitalRx is using artificial intelligence (AI), and machine learning procedures to lower manmade error and lowering in time for the processing of claim. Hence, the implementation of AI and ML technology into the flow of work is harnessing associations to steer down the cost of medical and rise the efficacy of the procedures of coverage.
Market Scope
| Report Coverage | Details |
| Growth Rate from 2025 to 2034 | CAGR of 9.17% |
| Market Size in 2024 | USD 613.17 billion |
| Market Size in 2025 | USD670.19 Billion |
| Market Size by 2034 | USD1,474,64 Billion |
| Largest Market | North America |
| Fastest Growing Region | Asia Pacific |
| Base Year | 2024 |
| Forecast Period | 2025 to 2034 |
| Segments Covered | Service, Service Provider, and Business Model, Regions |
| Regions Covered | North America, Europe, Asia-Pacific, Latin America, and Middle East & Africa |
Service Insights
Based on service, the specialty pharmacy segment accounted largest revenue share of 34% in 2024. The rapidly rising prevalence of rare and chronic diseases among the population is boosting the demand for the specialty drugs. The high prices of the specialty drugs are unaffordable by the majority of the patients across the globe. Therefore, the low affordability of the patients owing to the high prices of the drugs is a major factor behind the burgeoning demand for the pharmacy benefit management services to reduce the prices of these specialty drugs and make it affordable to the patients. These factors has led to the dominance of the specialty pharmacy segment in the global pharmacy benefit management market.
The benefit plan design and administration is anticipated to be the most opportunistic segment during the forecast period. The rising number of patients across the globe, opting for the medical insurance claims is fueling the growth of this segment. As per the India Express, people opting for medical insurance policy have increased from 30% in March 2020 to 80% in March 2021. Therefore, the rising number of people who opts for medical claims across the globe is expected to boost the growth of this segment significantly during the forecast period.
Service Provider Insights
Based on service provider, the insurance companies segment dominated the global pharmacy benefit management market in 2024. The rising number of acquisitions and mergers between the insurance companies and the pharmacy benefit management service providers is the major factor behind the dominance of this segment in the global pharmacy benefit management market. For instance, First Medical Health Plan, Inc. and Abarca Health LLC entered into a partnership for pharmacy benefit management services for three years. Moreover, the rising penetration of the health insurance companies across the developed and developing nations is further fueling the growth of the market significantly.
On the other hand, the retail pharmacy is expected to be the fastest-growing segment during the forecast period. The growing number of retail pharmacy units across the globe coupled with the rising penetration of the online pharmacies is expected to boost the growth of this segment. The rising penetration of internet, rising adoption of smartphones, and growing popularity of e-commerce among the consumers is fueling the growth of the online retail pharmacies, which is expected to boost the growth of the retail pharmacy segment in the forthcoming years. According to the International Telecommunications Union, about 64% of the global population had access to the internet and this number is expected to grow rapidly. The online pharmacies offers quick home delivery, convenient payment options, huge discounts, and easy refund and replacements. This is a major factor behind the augmenting demand for the online retail pharmacies. This is further expected to boost the growth of this segment in the global pharmacy benefit management market.
Country Level Insights
The pharmacy benefit management market has the United States as its leader since it integrates pharmacy benefits for 266 million Americans through 66 PBM entities, as reported by the National Association of Insurance Commissioners. As third parties, these entities link insurance companies with pharmaceutical producers to create better drug benefit plans while controlling costs. The ability of PBMs to unite health plan members into substantial networks provides improved pricing deals that help make prescription medicines more accessible and cost-effective throughout the U.S. healthcare system.
- In February 2024, Better Therapeutics Inc. entered into a rebate agreement with one of the biggest pharmacy benefit managers (PBMs) operating in the United States. The formal agreement allows commercial plan participants from a PBM to add AspyreRx to their formulary following rebate conditions.
Pharmacy Benefit Management Market Companies
- CVS Health
- SS&C Technologies, Inc.
- Anthem Inc.
- Medimpact
- Express Scripts Holding Company
- Benecard Services, LLC
- CaptureRx Inc.
- Change Healthcare
- OptumRx, Inc.
- Cigna
Government Announcement
- In February 2024, the New York State Department of Financial Services (DFS) superintendent proposed new market conduct regulations regarding Pharmacy Benefit Managers (PBMs) in New York State. DFS stated it expects the proposed regulations to help protect New Yorkers' access to prescription drugs, prohibit business practices that increase drug costs, and ensure that small independent pharmacies compete on equal footing with large pharmacies affiliated with PBMs.
Recent Developments
- In May 2025, HealthEZ, a national third-party benefits administrator, introduce EZrx, a next-generation pharmacy solution that leverages six cost-reduction strategies to deliver up to 50% savings compared to traditional pharmacy benefit plans. This solution supports self-funded plans by targeting high-cost prescriptions and optimizing pharmacy spend.
(Source: https://www.businesswire.com) - In November 2024, CerpassRx, a leader in pharmacy benefit management (PBM), announced the launch of the Intelligent Specialty Engine, an AI-enabled platform powered by Waltz Health to manage specialty drug spend. This intelligent marketplace ensures patients and payers receive the optimal combination of price, service, and clinical outcomes.
(Source: https://hitconsultant.net) - In May 2025, Waltz Health, a digital health company developing smarter, technology-enabled ways to price, distribute and prescribe medications, announced a new partnership with WellDyne to launch a transparent specialty pharmacy solution powered by Waltz Connect. WellDyne will leverage Waltz Connect's dynamic pharmacy marketplace and AI-driven routing engine to intelligently match prescriptions to the most cost-effective and clinically appropriate pharmacy, including WellDyne's own high-performing specialty pharmacy, HealthDyne.
(Source: https://www.businesswire.com) - In July 2024, Governor Josh Shapiro from Pennsylvania signed a bipartisan regulatory bill meant to control the behavior of pharmacy benefit managers (PBMs).
- In January 2023, Optum Rx Price Edge was launched to help buyers discover the lowest drug prices that exist on or off the pharmacy benefit. With this, leading service members can compare their on-benefit cost-sharing expenses to the available prices through discount cards.
- In April 2023, Cigna's pharmacy benefit management unit introduced a new pricing model, containing detailed rebate data due to rising U.S. legislative scrutiny on pharmaceutical middlemen's secrecy in drug pricing.
Segments Covered in the Report
By Service
- Specialty Pharmacy Services
- Benefit Plan Design & Administration
- Formulary Management
- Pharmacy Claims Processing
- Others
By Service Provider
- Retail Pharmacies
- Insurance Companies
- Standalone Pharmacy Benefit Management Providers
By Business Model
- Government Health Programs
- Employer-sponsored Programs
- Health Insurance Management
By Region
- North America
- Europe
- Asia-Pacific
- Latin America
- Middle East & Africa
For inquiries regarding discounts, bulk purchases, or customization requests, please contact us at sales@precedenceresearch.com
Frequently Asked Questions
Ask For Sample
No cookie-cutter, only authentic analysis – take the 1st step to become a Precedence Research client
 Get a Sample
Get a Sample
 Table Of Content
Table Of Content
 sales@precedenceresearch.com
sales@precedenceresearch.com
 +1 804-441-9344
+1 804-441-9344
 Schedule a Meeting
Schedule a Meeting