Healthcare Payer Network Management Market Revenue to Attain USD 15.83 Bn by 2033
Healthcare Payer Network Management Market Revenue and Trends 2025 to 2033
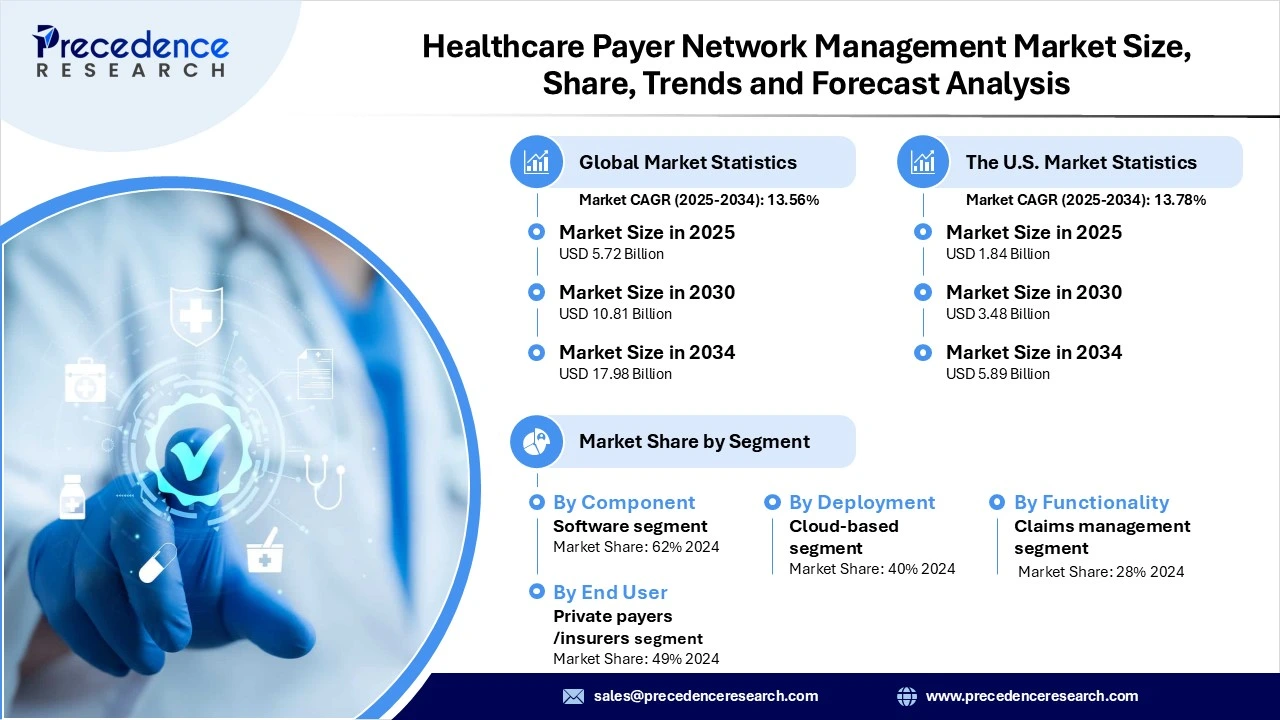
The global healthcare payer network management market revenue reached USD 5.72 billion in 2025 and is predicted to attain around USD 15.83 billion by 2033 with a CAGR of 13.56%. The healthcare payer network management market includes strategies, processes, and technologies that enable payers to build, optimize, and manage networks of healthcare providers. This market encompasses solutions for provider credentialing, contract management, compliance, analytics, and payment processing. Additionally, the shift towards value-based care, rising healthcare costs, and the growing demand for digital and Artificial Intelligence-driven solutions are leading to more coordinated care.
Segment Insights
- By Component, the software platforms segment held the largest market share, as it provides essential, centralized tools necessary for the digitization and efficiency required by modern healthcare systems. These tools enable better management of provider networks and facilitate effective data-driven solutions.
- By Deployment mode, cloud-based solutions led the market due to their enhanced scalability and improved data access. They streamline claims processing, enable fraud detection, facilitate telehealth, and remote patient monitoring, with enhanced care coordination by allowing secure access to patient data.
- By Functionality, the claims management segment holds the largest share of the market because it streamlines billing processes, reduces errors, improves reimbursement rates, and helps detect fraud by enabling value-based care.
- By End user, the private payers/insurers segment leads the market due to intense competition, rising healthcare costs, increased consumer demand for comprehensive benefits, and the strategic need to control expenditures using efficient network management tools.
Regional Insights
North America led the global healthcare payer network management market, driven by its advanced and high-expenditure healthcare system, which requires sophisticated solutions to manage complex provider networks and control costs. Additionally, the rapid adoption of advanced healthcare IT, including AI and cloud-based systems, is further supported by a shift towards value-based care and a complex regulatory environment that demands strict compliance. Government and regulatory bodies are increasingly promoting a shift from fee-for-service to value-based care models.
Asia Pacific region is projected to be the fastest-growing due to its large population, increased health insurance penetration, and rising healthcare expenditure. This growth is further heightened by rapid digital transformation, including the adoption of AI, cloud-based solutions, and telehealth. Government initiatives, such as India's Ayushman Bharat Digital Mission, along with increased public investment in digital health infrastructure, are accelerating market expansion. Additionally, strategic collaborations between local and global tech companies are driving innovation in claims processing and data management.
Healthcare Payer Network Management Market Coverage
| Report Attribute | Key Statistics |
| Market Revenue in 2025 | USD 5.72 Billion |
| Market Revenue by 2033 | USD 15.83 Billion |
| CAGR from 2025 to 2033 | 13.56% |
| Quantitative Units | Revenue in USD million/billion, Volume in units |
| Largest Market | North America |
| Base Year | 2024 |
| Regions Covered | North America, Europe, Asia-Pacific, Latin America, and Middle East & Africa |
Recent Developments
- In April 2025, HealthEdge introduced its HealthEdge Provider Data Management platform, which enables health payers to automate the critical task of maintaining accurate and up-to-date information on healthcare providers. This platform serves as a single source of truth for provider data, ensuring accuracy, consistency, and complete data lineage across all health plan operations while eliminating the need for manual reconciliation. (Source: https://healthedge.com)
Healthcare Payer Network Management Market Key Players
- Accenture Plc
- Aetna (CVS Health)
- Availity LLC
- Change Healthcare (Optum Insight)
- Cognizant Technology Solutions
- Genpact Limited
- HealthEdge Software Inc.
- IBM Corporation
- Infosys Limited
- Inovalon Holdings Inc.
- McKesson Corporation
- Medversant Technologies
- Optum (UnitedHealth Group)
- Oracle Corporation
- SAS Institute Inc.
- Tata Consultancy Services (TCS)
- TriZetto Healthcare Products (Cognizant)
- Verisk Analytics Inc.
- Wipro Limited
- ZeOmega Inc.
Get this report to explore global market size, share, CAGR, and trends, featuring detailed segmental analysis and an insightful competitive landscape overview @ https://www.precedenceresearch.com/sample/6722
You can place an order or ask any questions, please feel free to contact at sales@precedenceresearch.com |+1 804 441 9344